Introduction
Employee group insurance and corporate health insurance plans have become essential components of employer benefits programs in India, particularly following 2020. Organisations with more than 10 employees are required to offer a group medical insurance plan in accordance with IRDAI and ESI regulations. This transition signifies not only compliance but also the changing landscape of legal obligations and employee anticipations.
Why Group Health Insurance Is a Legal Essential
The social security framework in India is regulated by multiple interconnected laws:
- The Employee State Insurance Act of 1948 mandates coverage for employees in the organised sector with earnings up to INR 21,000 per month.
A. The employer contributes 3.25% and the employee contributes 0.75% of wages.
B. Addresses medical care, illness, injury, maternity, disability, family pensions, and funeral costs. - Insurance Act of 1938 and regulations set forth by the IRDAI
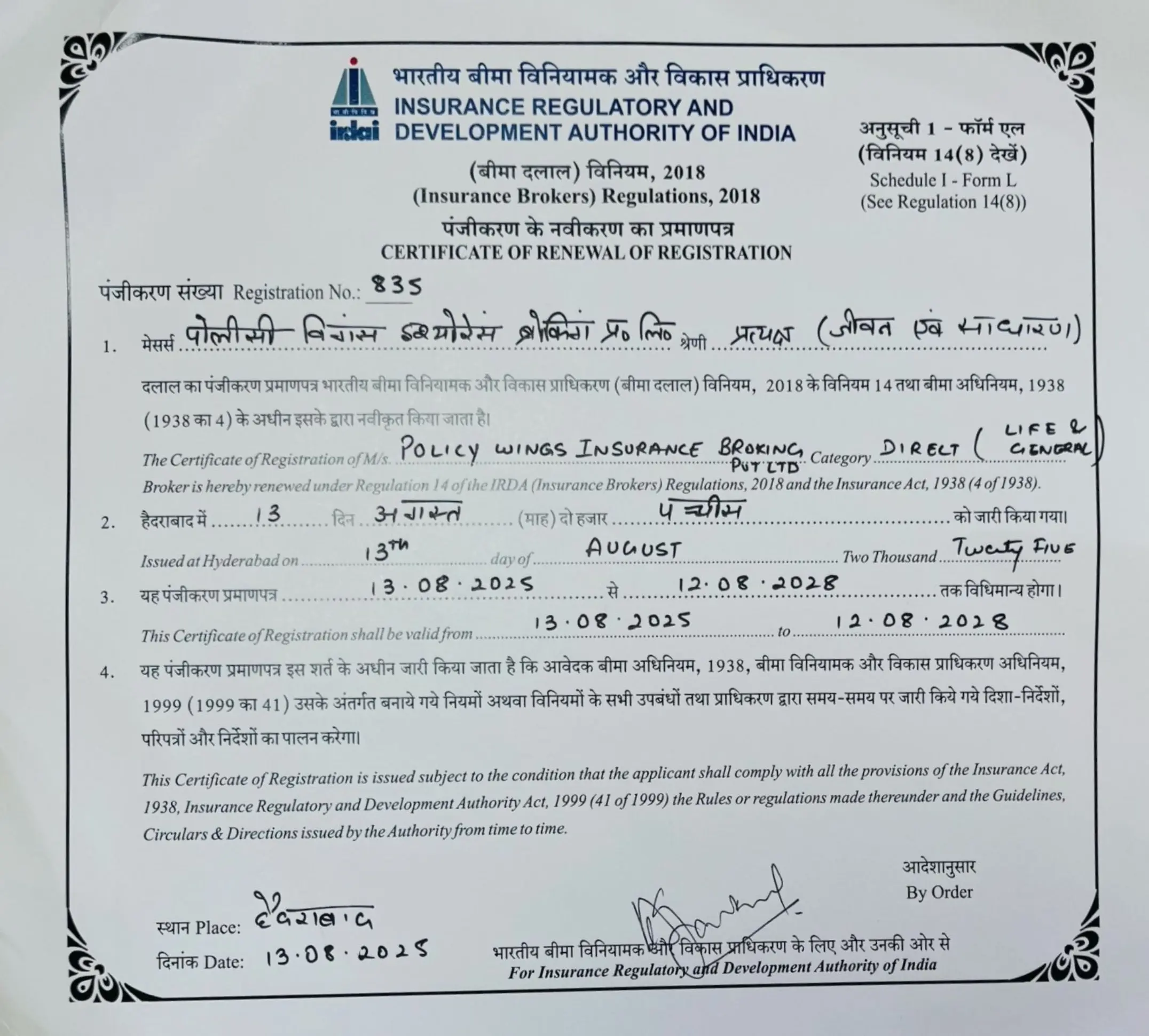
A. The IRDAI regulates the terms, pricing, and transparency of group insurance as stipulated in Section 34 of the Insurance Act.
B. On 1 April 2020, the IRDAI mandated insurers to implement affordable group health plans for organisations returning to operations after the pandemic. - Code on Social Security, 2020
Consolidates Employee State Insurance (ESI), Employee’s Provident Fund (EPF), gratuity, maternity benefits, and other related benefits into a single framework.
Mandatory Coverage: Who & What?
- Employers with ten or more employees not covered by ESI are required to provide group medical insurance in accordance with the IRDAI circular.
- Employers subject to ESI are not required to provide supplementary group plans as long as ESI coverage remains in effect.
- Employees with a monthly income exceeding INR 21,000, who are not covered by ESI, are legally required to obtain group health insurance (GHI) as an alternative.
Core Legal Obligations for Employers
- Obligations of care within common law and statutory frameworks
Employers are obligated to ensure workplace health and safety, a responsibility that is both implied in contracts and reinforced by legislation such as the OSH Code 2020. - Adherence to the terms set forth by the IRDAI policy
The IRDAI mandates disclosures regarding premiums, establishes timelines for claim settlements, and outlines channels for grievance redressal. Insurers are required to provide transparent contracts. - Consequences for failure to comply
Failure to offer required coverage may attract fines, imprisonment, loss of business licence, and reputational harm.
Important Differences Between Individual and Group Health Insurance
- Structure and cost sharing
- Group policies: employers pay all or part of the premiums; bulk bargaining can lower expenses.
- Individual: employee paid, with modifiable coverage.
- Scope of coverage
- Group: includes COVID-19 care, maternity, OPD, ambulance, hospitalisation, and pre-existing conditions (often immediate).
- Individual: may initially rule out pre-existing conditions; requires customised add-ons.
- Portability
Group health plans are subject to IRDAI portability rules, which provide continuity in the event of an insurer change.
Legal Precedents & Contractual Implications
- The UK Court of Appeal looked at implied employer duties in insurance benefit plans in Crossley v. Faithful & Gould (2004).
- Group insurance provisions must be explicitly incorporated into employment contracts in India, with any ambiguities being settled in the worker’s favour in accordance with the rules of contract law.
Best Practices for Implementing Group Health Insurance
- Clarity of eligibility
In employment agreements and policy wording, specify covered employees (permanent, contract, and trainees). - Sufficient levels of sum insured
In order to improve retention, take into account medical inflation and, if possible, include parent or family coverage. - When appropriate, smooth integration with ESI
Make sure covered employees are properly identified while avoiding redundant coverage. - Audits and policy renewals
Engage the finance, human resources, and legal departments in yearly reviews of the claims ratio, exclusions, and renewals. - Communication among employees and the resolution of grievances
As required by IRDAI, notify staff members of benefits and claim procedures and keep track of grievances.
Benefits and Strategic Importance
- Attracting talent and increasing productivity
According to studies, insured workers are more dedicated, take fewer sick days, and work longer. - Tax advantages
Employees benefit from Section 80D deductions for individual health plans, and premiums are deductible business expenses. - Social and moral accountability
Encouraging employee health is in line with Environmental, Social, and Governance (ESG) objectives and shows corporate citizenship.
Conclusion
Employee group insurance, backed by corporate health insurance plans, has transitioned from optional perk to legal imperative in India. The dual framework of ESI Act and IRDAI regulations compels organisations especially those with ten or more employees to implement robust health coverage mechanisms. Employers should view these not as merely statutory burdens but strategic tools to foster wellbeing, loyalty, and resilience.
Legal perspective:
- Create policies in compliance with the Code on Social Security 2020, the Insurance Act of 1938, and IRDAI guidelines.
- Include provisions pertaining to health insurance in employment contracts.
- To prevent statutory penalties, keep an eye on compliance.
- Make use of health benefits to boost output and brand recognition.