Introduction
In 2025 the prospect of group health insurance India is going through an essential transformation especially for startups which are progressively investing in startup insurance 2025 solutions customised to their all covered needs. Many of the converging factors containing regulatory reform, digital innovation, financial pressures and legal accountability are driving this trend.
Increasing Awareness and Market Motivation
India’s health insurance understanding has historically been less with only around 18% of urban and 14% of rural populations enclosed under any insurance scheme. Still stimulated by increasing healthcare costs and evolving expectations, the share of health coverage is projected to approach 50% by the end of 2025. The group health insurance India market has seen strong growth driven by increasing adoption of employee benefits programs and broader awareness of financial protection needs. For the startups contributing to group health plans is no longer optional as it’s become a strategic move to attract talent, maintain morale and reduce corrosion.
Digital Transformation and Startup Friendly Delivery
Technological benefit is remodeling how startup insurance 2025 is acquired and administered:
- Digital first claims and enlistment: Startups advantage from app based, paperless enlisting and claims settlement mechanisms that importantly decrease administrative friction.
- AI and telemedicine combination: Insurance providers now frequently bundle telemedicine coverage into policies, delegated by digital and AI tools that customise underwriting and hurtle up claims processing.
- Embedded and Insurtech models: Embedded insurance (coverage available within other digital workflows), wearable linked policies with behavior based incentives and real time data utilisation are gaining traction showcasing how startups can access flexible and modern group health insurance India plans.
Administrative and Policy Shifts Affecting Startups
Developing regulatory frameworks are both authorising and challenging for startups operating group health insurance:
- IRDAI’s deletion of the age bar: From 1st April 2024 the Insurance Regulatory and Development Authority of India (IRDAI) removed the upper age limit for buying health insurance policies and enlarging eligibility over all age groups.
- Precise oversight by National Health Claims Exchange (NHCX): In reply to rising healthcare costs in 2025 calculated at 13% which is more than the global average and the government is strengthening supervision over NHCX by engaging the finance ministry and IRDAI to limit overcharging and enhancing cost standardisation.
- Tax reform proposals: The GST Council and a government panel have given proposals to exclude health and life insurance premiums from the current 18% GST rate. If enacted then this could decrease the total premium load for startups and employees both alike but experts note that the effect may be silenced if not followed by structural changes.
- Influence of environmental factors: Premium hikes of 10% to 15% are being contemplated for residents in terribly polluted cities due to accelerating claim volumes which can signal how external risks are starting to factor into pricing dynamics.
Financial Availability by Innovative Financing
Health insurance costs continue to increase, posing various challenges, particularly for cash tied startups. New financial solutions are rising as the Premium financing by EMIs which states Fintech platforms are allowing startups to pay insurance premiums in attainable EMIs, ease the initial financial load and improve competitiveness/affordability of group health insurance plans.
Legal Regulatory Framework
Startups need to be aware of the legal and liabilities prospects aligned with group health insurance:
- Compliance with IRDAI regulations: Group health insurance plans have to comply with mandatory coverages (for example telemedicine), transparent grievance mechanisms and policy provisions under IRDAI frameworks any gaps in compliance can attract penalties or claim disputes.
- Claims oversight and treatment fairness: With centralisation of claims data via NHCX, discrepancies or inflations by hospitals may now be more easily flagged. Startups sponsoring such plans may be drawn into disputes over claims or pricing irregularities, adding managerial and legal oversight responsibilities.
- Fraud and rising of tech safeguards: Fraud still is a constant legal and financial risk. Technological interference such as blockchain relies on smart contracts or multi signature claim verification which can give powerful protection against fraudulent claims by making sure transparency and immutable records.
- Tax Involvements and responsibilities under Section 80D: Offering group health coverage mostly instigates tax advantages under Section 80D of the Income tax Act. However the startups have to make sure the proper compliance in documentation and deductions as failure could entice inquiry.
- ER responsibilities and liabilities: As employers the startups who finance group health insurance can be considered responsible for communicating policy terms, maintaining renewals and making sure the coverage continuity. No full information or failed renewals can open the door to legal or reputational consequences.
Why Startups Are Going for Group Health Adoption in 2025
Leading the threads together:
- Talent strategy: Group health insurance India policies help startups compete for talent with benefits typically available only in larger firms.
- Digital alignment: The seamless, digital first delivery of startup insurance 2025 fits the ethos and operations of modern startups.
- Cost and tax planning: decreasing admin costs, digital claims, GST reprieves and tax deductions can increase financial stability.
- Protection and increasing costs: Opposed to the element of healthcare inflation, cost increase due to pollution and systemic risk then the insurance protects both employees and startups.
- Regulatory preparation: Regulatory changes like IRDAI requirements and claims platform overlook structured group coverage more strongly which will be helping lower unmanaged disruptions.
- Fraud reduction by technology: Use of blockchain or smart contracts can lower risk, increase both legal compliance and investor confidence.
Conclusion
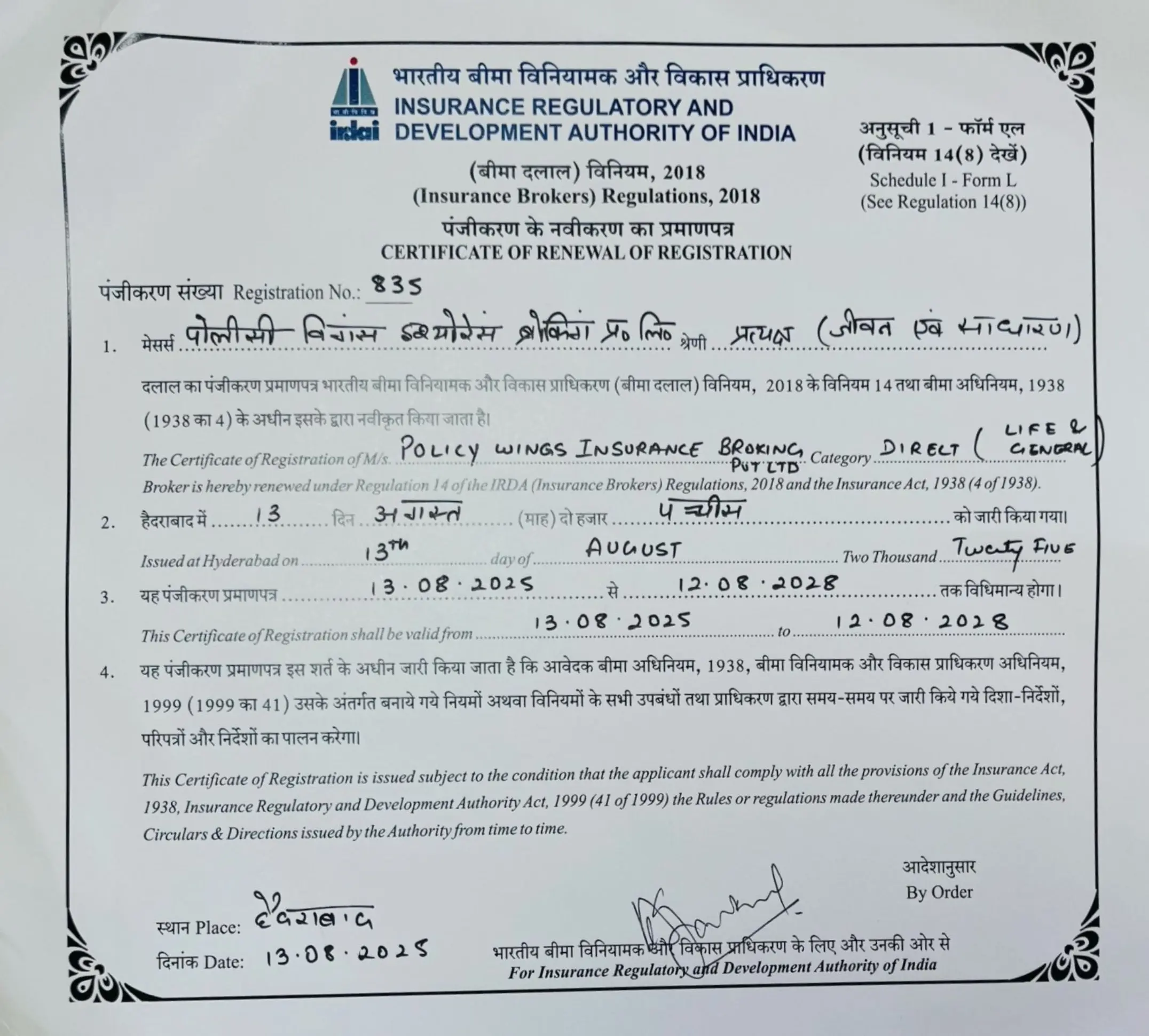
The year 2025 can mark an important point for group health insurance in India mainly within the startup insurance 2025 portion of domain. Controlled by digital innovation, regulatory evolution, financial necessity and legal prudence. Startups are rapidly adopting group health plans not only as perks but also as strategic tools to sustain growth, maintain trust and mitigate risk. For a firm like Policywings backing up such startups, placing group health insurance frameworks that are digitally enabled, regulatory compliant, affordable and fraud resistant will be supreme. By staying known to regulatory developments like GST exemptions, IRDAI mandates, NHCX governance and exploiting forward thinking tech the the startups can transform group health insurance from a cost particular into a competitive benefit while making clear governance and legal protection along the way.