Understanding Insurance: A Comprehensive Overview
Discover the importance of insurance, understand different types of policies, learn about coverage, claims processes, and even explore emerging trends in the industry.

Long ago, Chinese and Babylonian traders discovered a risk-reduction strategy that had never been employed before. Their entire group came to the consensus that we will pool some funds and divide losses equally amongst ourselves if anyone experiences a loss. The benefit of this is that everyone is risk-free for shorter periods. We continue to employ that concept today and call it insurance.
To put it simply, insurance is the collection of funds to eliminate risk for individuals. To clarify, the gathering of funds to address health-related risks is known as health insurance.
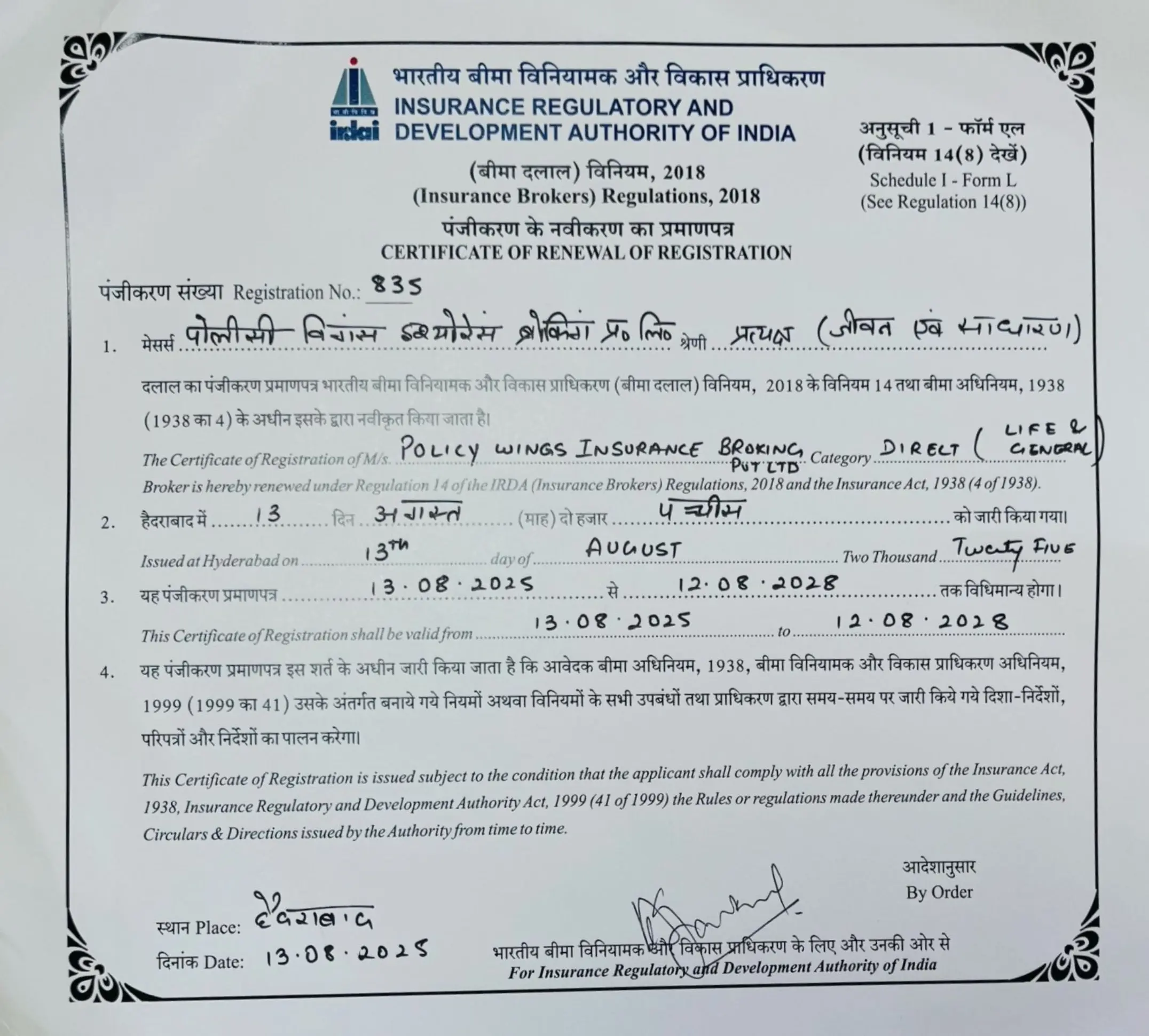
You cannot just hand someone your hard-earned money without any trust. Since, as you are aware, many people are affected by this and it occurs on a very large scale. This is where an insurance firm, comes into play, an insurance firm that has a good reputation is reliable, and complies with all laws and regulations, To ensure safe and high-quality services for the insured, an authoritative body is required to monitor the activities of insurance companies.
So here comes the IRDAI, The Insurance Regulatory and Development Authority of India (IRDAI) is the governing authority of the insurance sector in India. It is responsible for providing licenses and capital to establish insurance companies, as well as defining rules, regulations, terms, and conditions that must be followed for the validity of insurance contracts, including claim settlement, coverage, and product nomination.
Suggestions for the Policyholder
Read the policy and related documents carefully: Examine the terms and conditions of the policy in detail before accepting an insurance plan. Every insurance provider gives you the time to review the plan to finalize your decision.
Various Clauses in health policy!
Even though you may have paid significant premiums for your health insurance coverage, if you are unaware of its clauses then your claim might be partially or completely rejected when it comes to claiming the policy.
So, here are the clauses that everyone should know.
- Co-payment : So, a person buys a health insurance policy, and due to some reason he decides to claim the policy and the bill comes up for the payment. But the person thinks that the bill will be settled by the company itself but Some of the health policies (it is always advisable to the terms and conditions of the policy before buying) and the policy has a co-payment clause in it and this clause states that about 20% payment of the total bill amount must be paid by the policyholder and the rest 80% of the amount will be paid by the company. Co-payments are not required, and you are not the primary buyer unless you are elderly and suffering from pre-existing conditions. A co-payment provision can drastically cut premiums. As a result, this is not something you want in your insurance policy.
- Zonal Co-payment : Under this clause, the policyholder must treat his or her disease inside the policy’s specified zonal region, and if the policyholder does not meet this requirement, the insurance firm applies zonal co-payment in connected issues by the policy’s terms and conditions. This is due to the cost differences in medical facilities in different cities or places, which also influences the premium cost of insurance.
- Permanent Exclusions : Almost every policy company has some permanent exclusion, in such cases, policy companies do not settle the claim.
i) Adventures sports untoward
ii) Consumption of drugs or narcotics abuse
iii) Cosmetic surgeries
These are permanent exclusions and these expenses will not be covered by your health insurance.
- Permanent Exclusions : Almost every policy company has some permanent exclusion, in such cases, policy companies do not settle the claim.
- Waiting Period : Assume a person wants to get insurance coverage and signs up for it. Within the following 4 to 5 days, he is diagnosed with Asthma. In this situation, the insurer will state that the waiting time is one year from the commencement of the insurance. Hence, from one year beginning with the policy’s commencement, the policyholder’s claim would not be accepted; this is what a waiting period is! It also has an impact on the insurance policy’s premium cost.
- Room Rent Restrictions : Some insurance policies will state that most services given in your room, such as doctor’s fees, consultant fees, or any other diagnostic expense, are not covered. They will not be completely covered if you choose a room that is larger than the room limit specified in your policy. Assume that under an insurance policy, the room rent maximum is plainly stated to be rupees 10,000, but he decides to pay a room rent of rupees 20,000 instead. Everything is on his bill, the room rent, doctor’s charge, consultation cost, etc., therefore only half of the bill is covered by the insurer and the other half must be paid by the policyholder.
Cashless Claims : To understand a cashless claim, we have to understand it into the two different parts :
1) Planed Treatments/pre-authorization: In this instance, if you wish to file a cashless claim, you must do the following:
- You must notify the hospital of your surgery, etc., at least two to three days before the case is determined, and along with this, and at the same time you must also visit the insurance desk at the hospital, which is part of the specific insurance company network.
- Submit documents like Insurance copy, Identity proof, Initial Diagnostic Report, and related documents if asked by the insurance desk.
2) Emergency Situations : In case of emergencies, whenever the patient is been admitted, within 24 hours from the date of admission, you have to intimate the same to the insurance company. If you don’t do so then it will be more of a reimbursement case rather than a cashless claim.
7. Reimbursement : If your policy requires you to file a reimbursement claim, you must do so within 15 to 30 days after the date of discharge of the patient (The number of days may vary depending on your insurance provider).The claim procedure may be commenced offline or online. Along with the filled form, attach the following :
-Original reports
-Original copies of the hospital bills
-Doctor’s consultation reports
-Diagnostic reports
-Any other document if required.
8. Claim Settlement period : The insurance provider must either settle the claim or reject it within 30 days of the final document submitted for the claim.
What if your claim is rejected?
- Send an email describing the problem to the grievance redressal department.
If the response is not received within 15 days or if the response is unsatisfactory, then
- Approach to the insurance ombudsman. (an ombudsman is a mediator between the insurance company and the policyholder)
If the ombudsman’s response is unsatisfactory as well, then
- You must approach the IRDAI (Insurance Regulatory Development Authority of India)
- Call on 18004254732 OR Email complaints@irdai.gov.in
Related Posts
FAQs
Insurance traces its historical origin to the practices of Chinese and Babylonian traders who discovered a risk-reduction strategy long ago. They pooled funds and agreed to divide losses equally among themselves if anyone experienced a loss. This innovative approach allowed them to reduce individual risk for shorter periods. This concept, which continues to be employed today, is known as insurance.
An insurance firm plays a crucial role in the insurance industry. It acts as an intermediary that collects funds from policyholders and provides coverage in case of specified risks. It ensures that the collected funds are managed efficiently and used to cover claims when necessary. A reputable insurance firm is essential for ensuring trust and compliance with laws and regulations, ultimately safeguarding the interests of policyholders.
The Insurance Regulatory and Development Authority of India (IRDAI) is the governing authority of the insurance sector in India. Its primary responsibilities include providing licenses and capital to establish insurance companies, defining rules, regulations, terms, and conditions for insurance contracts, and overseeing activities related to claim settlement, coverage, and product nomination. The IRDAI ensures that insurance companies operate within the framework of established regulations to protect the interests of policyholders.
Here are some key suggestions for policyholders:
- Read Policy Documents Carefully: Examine the terms and conditions of your insurance policy thoroughly before accepting it. Take your time to review the plan to make an informed decision.
- Understand Policy Clauses: Be aware of the clauses in your health insurance policy, as not understanding them can lead to claim rejections. Familiarize yourself with co-payment, zonal co-payment, permanent exclusions, waiting periods, room rent restrictions, and other clauses.
- Cashless Claims vs. Reimbursement: Understand the process for cashless claims and reimbursement. Follow the specific steps for planned treatments and emergency situations to ensure a smooth claims process.
- Claim Settlement Period: Be aware that the insurance provider must settle or reject your claim within 30 days of receiving the final documents.