Health Insurance TPA
Health Insurance TPA
An unexpected medical situation can be difficult for the whole family. All you would want is for your relative to receive medical care without having to worry about money.
However, only if all the paperwork is completed correctly, which may seem like a bother at the time, can health insurance assist to cover these medical costs. TPAs can help you in this situation.
What Is a TPA or a Third-Party Administrator?
An individual or business that assists in the processing of claims made under a health insurance policy is referred to as a TPA or third-party administrator.
They are unaffiliated third parties that the insurance company may use to help resolve disputes. TPAs essentially act as a link between the insurance company and the policyholder.
The range of coverage under health insurance is broad, and the claim-settlement procedure includes internal processing and verifications.
On behalf of insurance companies, TPAs monitor the work involved in resolving health insurance claims and uphold the standard of services. In conclusion, TPAs handle the payment of your medical claims and hospital expenses.
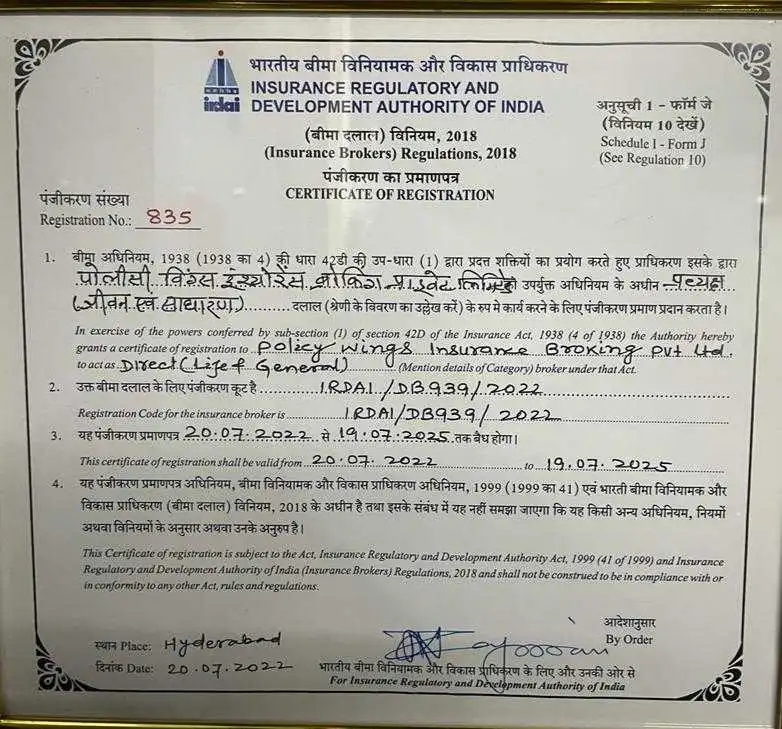
The Insurance Regulatory & Development Authority of India (IRDAI) issues licenses to all TPAs. One TPA can also be connected to several insurance providers simultaneously.
TPA’s Relevance in Health Insurance
The hospital bills and other expenditures will be taken care of by a Third Party Administrator. You may just take care of them when the illness of a family member or friend is upsetting you. The TPA will handle everything else.
The TPA is your one-point contact for all service-related issues. Their primary responsibility is to handle claims. However, they have other responsibilities listed as a part of their KRA as well.
Each TPA company has a contract with the concerned insurer regarding their roles and responsibilities listed in their SLA (service level agreement). The role of a TPA is to provide better service to the policyholders since the insurer is unable to open offices at smaller locations. Hence they engage in multiple TPAs in various locations to provide service and claim assistance to their customers.
For you, as an insured or a policyholder, TPA is your link with the insurer. In conclusion, we may say that TPA is pertinent to:
- Extensive expertise in healthcare services.
- Enhance the standard of services.
- Manage and look into the allegations.
- Pay attention to the Cashless and Reimbursement TAT (Turn around time).
Important information about TPA’S
The following are some crucial TPA-related details that you should be aware of:
- It is crucial to realize that insurance companies have the right to revoke or modify TPA agreements at any moment. The insurance provider is the main point of contact, so if a policyholder needs further information, they should get in touch with them immediately.
- However, for health insurance plans, the IRDAI gives policyholders the option of selecting their favourite TPA.
- The insurance company needs to keep their policyholders informed about the TPAs that are currently working for them and any modifications or replacements that take place. The insurance company might direct you to contact the current TPA when you file a claim.
Benefits of Third-Party Administrators for Health Insurance Companies
Smooth health insurance claim settlement is one of the main advantages third-party administrators, or TPAs, provide to health insurance companies. For health insurance businesses, TPAs also offer the following significant benefits:
- A dedicated source that facilitates claim settlement.
- Coordination from the start of treatment to discharge.
- Proper administration & examination of claim requests.
- Superior service quality.
Do all insurers have TPAs?
Most health insurance companies have a TPA to handle their operations. However, some new-age health insurance companies have their own in-house TPA services wherein the claim is also handled by them in-house without involving a third-party administrator.
To handle the claims process, many insurers today have their own internal divisions, notably for the retail health portfolio. However, the TAT and other amenities become crucial differentiation factors for insurance on the claims management front. Building an internal claims procedure enables the insurer to occasionally offer exceptional benefits to policyholders.
The role of a TPA is limited to operational activities only. For example, TPAs are only permitted to handle claims; they are not permitted to make decisions about them. Therefore, in a difficult case, a TPA may not be able to handle escalations wherein the insurer needs to step in. TPA’s have their internal guidelines for handling standard claims. However, in some situations, they might resort to the insurer for assistance in a special case. Therefore, a claim procedure that is handled internally by the insurance company, as opposed to using a third-party administrator (TPA), is usually simpler and quicker.
However, most insurers are inadequate in handling the entire claim services on their own. Hence they need the help of a large organization with offices in multiple locations to handle their services and be the POC (point of contact) of their customers.
TPAs rely on the insurer to help policyholders with their health insurance claims. As a result, a TPA’s effectiveness is based on how stringent its rules of operation are and how precisely the health insurer defines the protocols they must follow in order to handle the claims they receive.
Multiple TPA registration for a single insurer:
When someone uses the phrase “multiple TPA registrations for a single insurer,” they often mean that more than one Third Party Administrator (TPA) has registered with or collaborated with the same insurance provider.
Multiple TPA registrations for a single insurer may be necessary to spread out the workload, make use of each TPA’s unique expertise, improve customer service, or guarantee redundancy in case one TPA experiences problems.
- Employing several TPAs for claim processing:
An insurer might work with many TPAs to fulfill administrative and claim-processing duties for various business lines or areas. With this strategy, the insurer may take advantage of various TPAs’ skill sets and efficiency in particular fields. - Different TPAs for diverse insurance products:
Insurers occasionally utilize various TPAs for the various insurance products they provide. For instance, one TPA may concentrate on processing health insurance claims, while another would concentrate on handling vehicle insurance claims. - Numerous TPAs for redundancy:
As a backup plan, some sizable insurers may decide to have numerous TPAs. The insurer can rely on a different TPA to maintain continuity in claim processing if one TPA runs into technological or other difficulties. - Regulations:
To promote competition or guarantee that insurers have the resources to handle claims efficiently, insurance authorities in some areas may mandate or permit insurers to have numerous TPA registrations.
Role of TPA in the insurance industry in India:
TPA’s primary role is to handle the claim settlement end-to-end. However, they have other responsibilities as well, which could listed as:
- Provide insured people with their health cards and administrative assistance:
Now that you understand what a health insurance TPA is, you can see that one of its key responsibilities is to manage all client information in both online and offline records in an organized manner.
As soon as the insurance policy is in your name, the insurer will provide a copy of the insurance form and any other pertinent documentation to the TPA of your choice for them to review. During the renewal process, the insurance policy is updated and given to the third-party administrator for processing.
It is then the responsibility of the TPA to maintain and update these records on a regular basis. - Claim Verification:
The TPA will receive the claim form and the information that you have provided to them when you file a claim with your health insurance company.
It is important to keep in mind that the TPA will examine all of your medical bills, the documentation that is provided, and the claim form to ensure their validity. To ensure that the insurance claim is valid, they may even call the hospital where you are admitted or where you are planning to receive treatment in order to confirm the validity of the claim.
It is possible that they will contact you and the insurance company to confirm the information they have provided.
How to TPAs help in Claim Settlement?
A third-party administrator (TPA) is responsible for determining if a health insurance claim is valid or not. According to the manner in which you select for the settlement of your claim, this is the way in which they handle it.
When a scheduled or unexpected cashless hospitalization occurs, they work closely with your preferred network hospital and take care of paying the hospital expenses on your behalf. As soon as they receive all of your paperwork, they will send it to the hospital in your network, and they will handle the insurance claim for you.
During the investigation process and working with the hospital, they verify the validity of your insurance claim and the supporting documentation before reimbursing you for your expenses as soon as possible.
- Set up Value-Added services:
A TPA also aids in setting up other value-added services like ambulances, wellness programs, etc. along with their primary role of claim settlement. - Helpline Service:
It should be noted that TPAs are the main point of contact for clients who have insurance coverage. When the insurer is unable to resolve your health insurance concerns and questions, you will be referred to your selected third-party administrator (TPA).
Third-party administrators are well-equipped to handle your problems and provide you with practical solutions to them.
Their customer service department is available to assist clients 24 hours a day, 7 days a week. Additionally, the TPA for health insurance can also offer a number of other services, such as emergency ambulance services, wellness initiatives, illness management programs, and other services related to illness management. They sometimes have an effective website or mobile application as well to facilitate claims. - Makes the hospital networks stronger:
Having a TPA is a crucial component of utilizing the benefits of health insurance coverage. It also creates a robust network of hospitals wherein the policyholders can receive medical care. The TPA works to assemble the best hospitals that can quickly set up cashless and permit fee negotiations.
How Does TPA Help Policyholders?
The TPA streamlines the claims process for health insurance policyholders by simplifying the process of filing a claim.
Depending on the type of claim, either a cashless or reimbursement process can be used. In the event of a medical emergency, the insured will visit a hospital in order to receive medical care. In order to qualify for reimbursement, the patient must be hospitalized for at least 24 hours in order to make a claim (and not for daycare operations like cataract surgery or treatment for another condition on the list).
In this scenario, the policyholder will notify the TPA or insurance provider of the hospitalization and the treatment that will be needed.
In case a cashless treatment is feasible, the TPA will then get in touch with the hospital and request permission for a cashless treatment to be provided. In the event that reimbursement is not possible, the claim will be handled for reimbursement.
In the event that the request for cashless treatment is accepted, the hospital will send any relevant medical invoices regarding the procedure to the TPA following the procedure. It is likely that the policyholder will be asked to produce the documentation later on if the request is denied.
It is the TPA’s responsibility to carefully examine the invoices and other documentation before starting the procedure of settling the claim. In the event of cashless claims, the hospital will handle the payment directly, whereas, in the event of reimbursement claims, the hospital will receive payment through the insurance company on behalf of the patient.
How do TPAs work in India?
TPAs, or third-party administrators, are crucial in streamlining the claim-settlement process for health insurance providers and consumers. TPAs take on significant duties for health insurance providers to help policyholders, whether it be with cashless claims or reimbursement claims. Let’s clarify how TPAs function in these two scenarios.
- Cashless Claim Settlement:
A policyholder contacts their health insurance company’s TPA when they wish to opt for cashless treatment. The TPA provides assistance in selecting the best network hospital for medical care. The TPA provides guidance to the policyholder at the hospital desk when they arrive for treatment on the filing of the necessary vital paperwork. The TPA pays the hospital for the cost of the treatment after receiving approval for it.
Basically, TPAs work on behalf of the insurer and become the only point of contact for the policyholders. - Reimbursement Claim Settlement:
For any reason, the policyholder chooses to visit a hospital that is not in the network. They make their decision known to the TPA, receive treatment, and cover hospital expenses.
After being released from the hospital, the policyholder submits a claim to reimburse the hospital bills they paid. Here, the TPA provides the policyholder with a list of crucial papers that must be presented in order for a reimbursement to be approved. Following claim acceptance, the health insurance provider deposits the claim payment into the policyholder’s designated bank account.
Cancellations of TPA in Health Insurance:
The insurance company selects the TPA; the TPA does not have any influence over whether it is hired or fired. However, a policyholder has the option to revoke the current TPA and ask the insurance provider for a different TPA.
Steps to terminate your TPA for health insurance, follow the instructions below:
- Make contact with your insurance provider via phone or email.
- Share your insurance’s specifics, including your policy number.
- Request for termination of the current TPA, along with the rationale.
- The request for cancellation will either be accepted or declined by the insurance company.
- Select a different TPA with an IRDAI license if approved.
Ideally, a TPA should facilitate the claims and other services. However, if they are not being able to assist or are uncooperative, the policyholder has the right to ask for a change of the TPA, provided there are other TPAs in his location.
Whom Should You Contact About TPA Service Issues?
The insurance regulator has now given customers the option to select the third-party administrator (TPA) from a list of those hired by the insurance firm in an effort to expedite the claim-handling procedures for health insurance. The policyholder may select a different TPA if the insurer terminates the TPA’s services. At the time of renewal, the policyholder will have the option of switching TPAs.
If a policyholder doesn’t select a TPA of his choosing, the corporation will choose one for him. The policyholder will, however, be forced to continue with that TPA if the insurer uses the services of only one TPA. The regulator has emphasized that the insurer might limit the number of TPAs from which the policyholder may select based on the health insurance service and the policyholder’s geographic region.
Conclusion
It is essential for an insurer to be able to move through the process of obtaining health insurance quickly and smoothly with the assistance of a TPA.
It is they who are the megastars in the background who manage the on-stage performance that takes place on the stage. When it comes to choosing your health insurance TPA, it is just as important as picking your insurer since you will be entrusting them with your personal health care.
Frequently Asked Questions
No! After a health insurance provider issues a policy, TPAs begin to play a part in the process.
TPAs manage a range of duties for insurance companies, including enrollment, premium collecting, claims processing, and customer support. They serve as a point of contact for the policyholders and the insurance company. A corporation that provides health insurance plans to individuals, families, or groups is known as a health insurance provider.
In conclusion, TPAs give administrative assistance to health insurance companies, whilst these companies cover policyholders' medical bills.
According to recent studies, this approach could be viable. Please talk about this with your insurance provider.
The TPA team may include professionals in the following disciplines: physicians, insurance advisors, lawyers, information technology (IT) specialists, etc.
The health insurance provider hires the TPA to help with the claims processing procedure.
Leading Health Insurance Companies